Kidney Transplant
The Kidneys
The kidneys are a pair of vital organs that perform many functions to keep the blood clean and chemically balanced. Every day, your kidneys process almost 190 liters of blood to filter out about 2 liters of waste products and extra water. The kidneys then process the filtered waste by-products into urine.
End-stage renal disease (ESRD)
Every year, over 12,000 Filipinos develop End-Stage Renal Disease (ESRD). ESRD occurs when the kidneys are no longer able to function at a level needed for day-to-day life. It usually happens when chronic kidney disease (CKD) has worsened to the point where kidney function is less than 10% of normal. The most common causes of CKD are uncontrolled hypertension and diabetes.
Kidney Transplant–Best Treatment Option for ESRD
Often, the best treatment option for ESRD is a kidney transplant where a patient (recipient) receives a healthy kidney from a donor. Kidneys for transplantation can come from either a deceased or living donor.
Benefits of Kidney Transplant
A successful kidney transplant has many benefits. These include:
- Freedom from long-term renal therapy
- Increased energy
- Fewer, if any, diet and fluid restrictions
- Better quality of life
- Return or having a close to normal lifestyle
- Ability to return to work and lead a full life
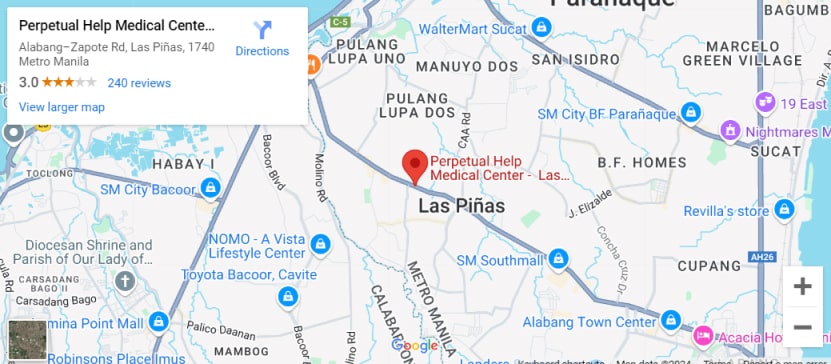
Why Go to the Perpetual Help Medical Center – Las Piñas (PHMC-LP) Kidney Transplant Unit (KTU)?
The Perpetual Help Medical Center – Las Piñas (PHMC-LP) Kidney Transplant Unit (KTU) provides the best possible care to kidney transplant patients and their family. Our mission is to make the entire kidney transplant process easier and less stressful for the patient.
The KTU has a multidisciplinary team of medical and surgical specialists who utilize state-of-the-art diagnostic and therapeutic equipment. The KTU Team is highly trained to provide the following services: